Lip Filler Injections – the new protocol
Lip Filler Injections – the new Ultrasound-Guided protocol.

AADFA International, outlines how to perform Lip Filler injections that are compliant with the new clinical & legal standard. This is the second in a series of articles drawn from recent AADFA presentations as the only Dentists ever invited by the Australasian Society of Aesthetic Plastic Surgeons to speak at their annual Non-Surgical Symposium.

In the last AADFA news article, we outlined the importance of dental practitioners now only performing injections of Botox and Dermal Filler while under ultrasound guidance, for improved safety and efficacy.
Advances in portable, wireless ultrasound technology, combined with the development of clear and easy-to-follow clinical protocols by AADFA, meant that ultrasound guided facial injections now set a new clinical and legal standard which responsible practitioners would be expected to follow and the only way in which they ought to continue providing such services.
Indeed, there has been repeated confirmation from healthcare regulators that they would view a failure to utilise such easily accessible imaging protocols during Botox and Dermal Filler procedures, as a failure to take all reasonable steps to ensure patient and procedural safety. This would be considered to fall substantially below the level of care expected of a responsible dental practitioner, exposing them to regulatory action and even patient litigation in the event of sub-optimal outcomes or complications emerging that could otherwise have been avoided. Additionally, a failure to disclose to patients that a method of visualisation exists which would make procedures safer and more effective, would undoubtedly mean a failure to gain informed consent.
This series of clinical articles, highlighting how dental practitioners should now look to utilise ultrasound guidance for facial injectable procedures, commenced in the last edition looking at the injection of Botox into the Masseter muscles. In this article, we review how ultrasound guidance can improve the clinical outcomes from dermal filler lip enhancements, while at the same time, making them safer.
What was wrong with the old way of injecting Dermal Filler in Lips?
The problem with the old way of injecting Dermal Filler was that it was, essentially, a blind injection, based purely on presumption; a practitioner’s generic knowledge of textbook anatomy; and largely unreliable, subjective physical examination. Given the extreme variation and complexity of individual facial anatomy, injecting blindly is far from ideal, with research showing this issue of unpredictable, blind technique, being solely responsible for the occasional serious complications and poor clinical outcomes experienced from an otherwise safe and reliable treatment modality.
While the lips may seem like uniform structures, their internal anatomy can be quite complex and variable, with them also inhabiting a position intimately entwined with several other key facial structures, meaning they influence not only the aesthetics of the lower face, but vital functional aspects, ranging from expression and speech, through to mastication and proprioception. It is a failure of the practitioner to be able to truly understand the individual anatomy of a patient’s lips, especially in relation to the precise location of the labial arteries, that has been shown to directly impact the safe and effective delivery of dermal filler injections.
With the number of dermal filler lip treatments being performed growing exponentially over the last decade, so too has the frequency of complications experienced. As a direct result of the limitations of a blind approach to treatment, three main iatrogenic side effects have been frequently reported following dermal filler lip injections:
- Vascular Occlusion / Skin Necrosis

With the high vascularity of the lips and facial soft tissue, the most dreaded potential complication of any injection of dermal filler, is that of vascular occlusion, where the implanted filler gel compromises blood supply, leading to sequelae which may include tissue necrosis, secondary infection and scarring. The mechanism by which dermal filler gel can cause vascular compromise is either by inadvertent direct intravascular injection, or by compression of the vasculature resulting from pressure exerted by adjacent filler in the tissues. Regardless of the mechanism, vascular occlusion is a serious condition which presents aesthetic, functional and psychosocial issues for patients and requires active emergency management.
While practitioners have previously tried their best to mitigate the risk of this complication by diligently studying textbook anatomy and being guided by the typical patterns of the labial arteries dissected in cadaveric studies, there was simply no way to know for sure where these vital vascular structures lay, in reality, for the individual patient about to receive the treatment. Practitioners, despite their best efforts, previously had no choice but to fly blind!
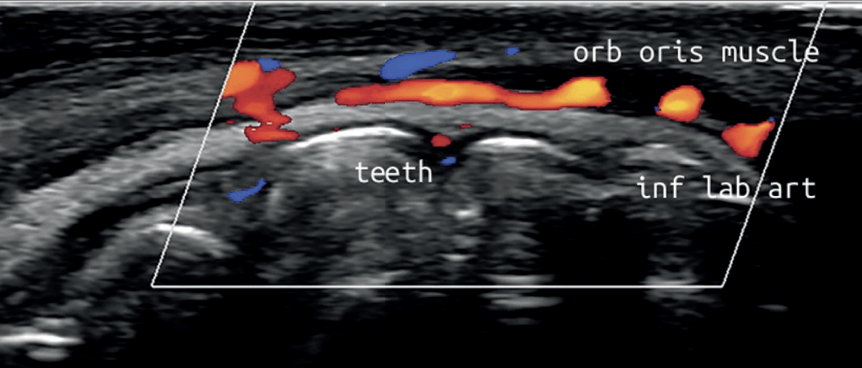
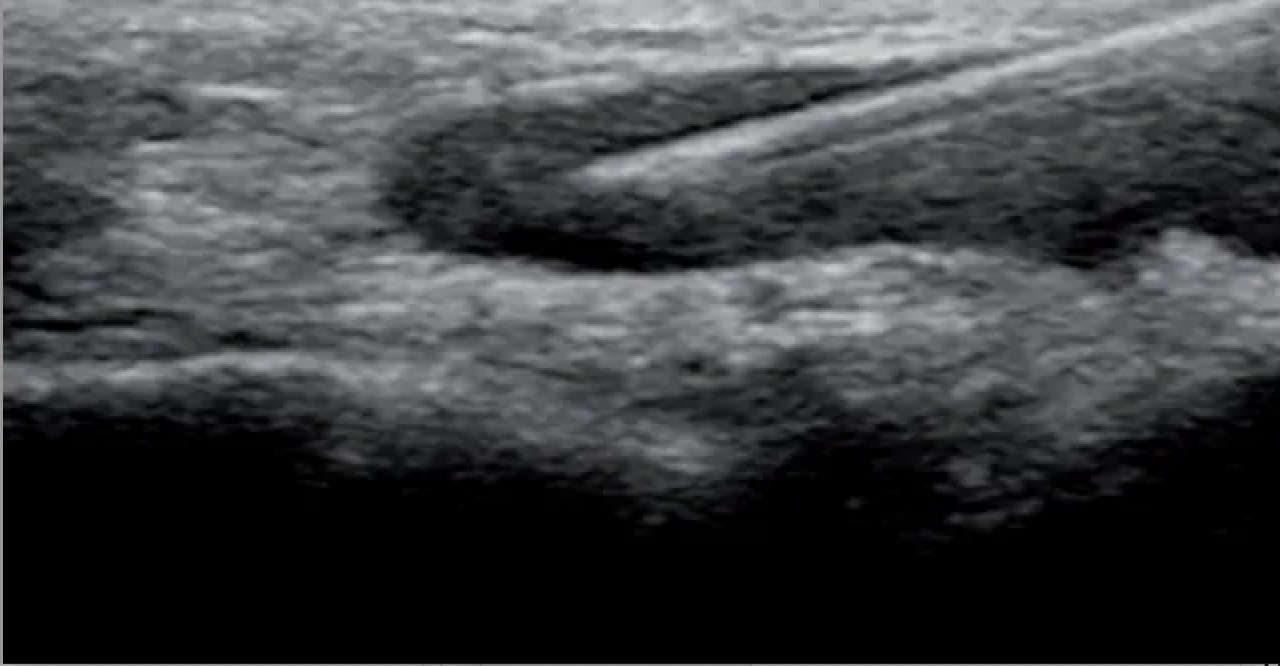
While research and texts have traditionally claimed that a superficial plane in the lips was a safe approach, given, in most cases, the labial arteries transverse a deeper plane, below the orbicularis oris muscle, recent ultrasound studies of living individuals have shown there to be far more variation in the location, size, orientation and trajectory of the labial arteries than previously thought. Indeed, in more than a third of patients, the labial arteries lie above the muscle, in areas traditionally believed to be safe, and in many patients these structures switch tissue layers frequently in their journey across the lips.
2. Lumps / irregularities

Non-inflammatory lumps are the most common complication seen after dermal filler lip injections. While not usually causing the patient discomfort or functional issues, they certainly create aesthetic and psychosocial challenges.
To achieve the best clinical outcomes from dermal filler placement in the lips, injecting into the orbicularis oris muscle layer needs to be avoided, especially in the region of its attachment to the overlying dermis, and deposition of the product needs to be as consistent as possible. Filler placed intramuscularly or in the incorrect tissue plane, will tend to clump and distort during normal lip function and muscle contraction.
Such accuracy, when working within thin lip tissue, is rarely able to be achieved, even by experienced injectors, when performing injections in a blinded fashion. Without the ability to directly visualise the precise anatomical location of your needle, traversing different tissue layers is practically inevitable as they cannot be readily discerned clinically.
This is especially true if a practitioner is using a blunt cannula rather than a needle. Ultrasound studies have shown that dermal filler placed using a blunt cannula in lips, results in a far more inconsistent deposition, with the cannula regularly passing too deep and entering muscle layers, increasing the risk of post-operative lumps and irregularities.
3. Filler Migration

Dermal filler migration, predominantly a spreading of product across the vermillion border into the white lip, is an increasingly common problem, which has a significant aesthetic and psychosocial impact on patients.
The rise in this complication can be directly attributed to the use by inexperienced practitioners of “fad” injecting techniques – like the “Russian technique” – which displays a fundamental lack of understanding and respect for natural lip anatomy.
The “Russian technique” creates a series of vertical channels, puncturing down through the vermillion border, into the body of the lip vermillion. Unfortunately, breaching the integrity of the dermal attachment of the orbicularis oris muscle in this way; which would usually contain filler within the lip itself; permits filler to spread along a path of least resistance, across the lip border and on into the white of the lip, compromising definition and establishing a problematic lip thickening.
Additionally, this method, as with the routine use of blunt cannula instead of needle for lip enhancement, invariably results in filler being injected too deep, beneath the orbicularis oris muscle. In this position, during normal lip function, muscular contraction forces filler to spread through natural deep tissue layer communications to the white lip, leading to the same risk of filler migration, but in this case, causing more of a “duck bill” appearance.
No matter how experienced a practitioner thinks they are, this risk can only be avoided by ensuring filler is placed in appropriate and favourable anatomical positions with the use of ultrasound guidance.
So, what is the new protocol?
In line with the new regulatory and legal standards which are now in effect, dental practitioners are ethically and legally obliged to utilise the safest approaches to treatment available and to minimise risk. Portable, wireless, hand-held, ultrasound technology must now be used in the dental clinic to allow direct imaging of individual lip anatomy both before and during the injection of dermal filler, in the same way that dental x-rays are used routinely to diagnose; guide treatment; and avoid complications.

Practically, ultrasound must now be used by Dentists looking to perform lip filler injections in two ways:
1.
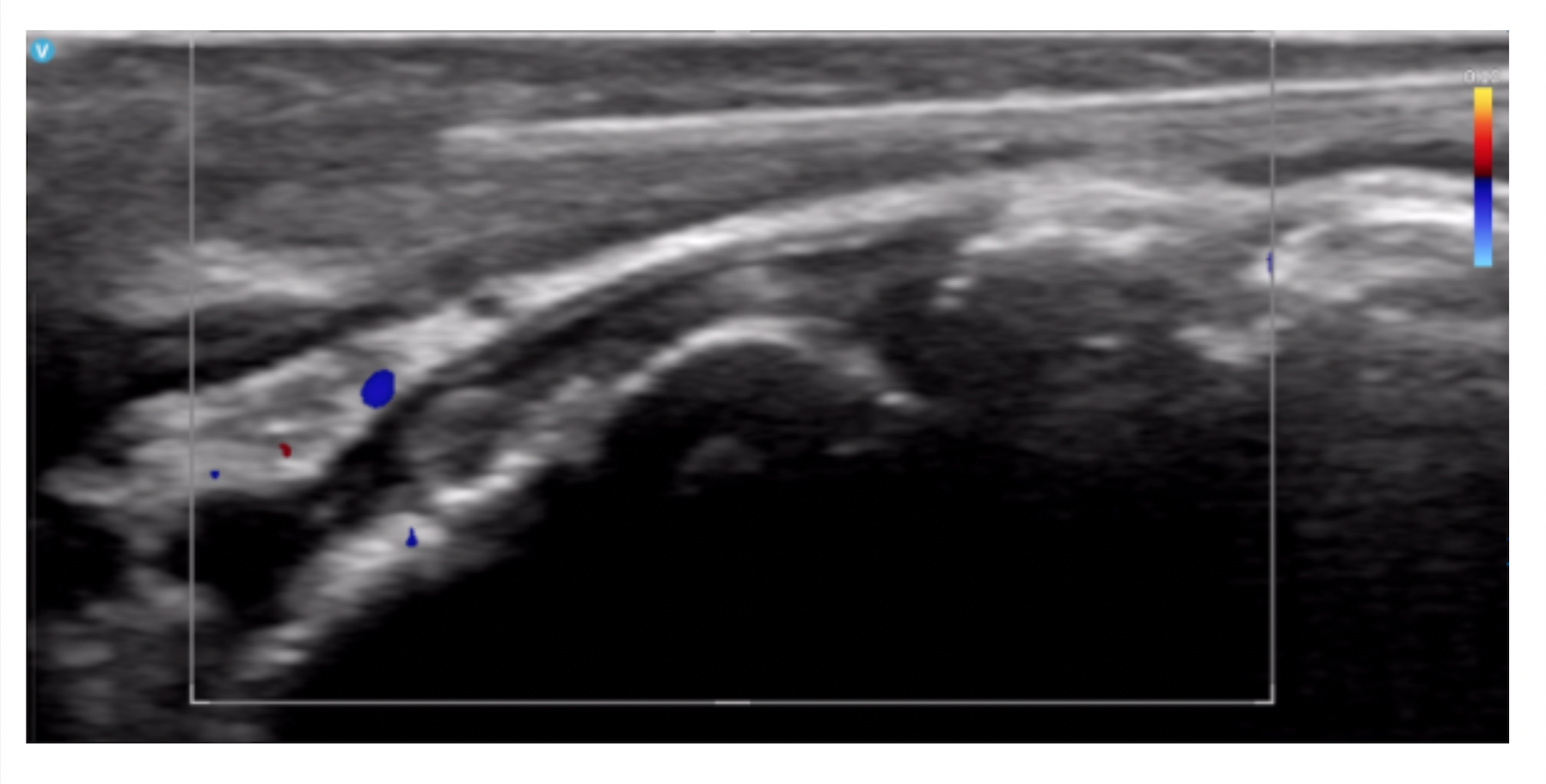
An ultrasound analysis must be recorded during the examination/consultation prior to performing the injections (Fig.6.). This allows the practitioner to evaluate the precise location, orientation and pathway of the labial arteries in each individual, as well as determining the most appropriate depth and tissue plane in which to inject the filler, rather than relying on a generic hypothesis of where these structures may be located. From this pre-treatment analysis, an appropriate, individualized, injection plan can be developed in relation to the site; depth and dosage of dermal filler injections required.
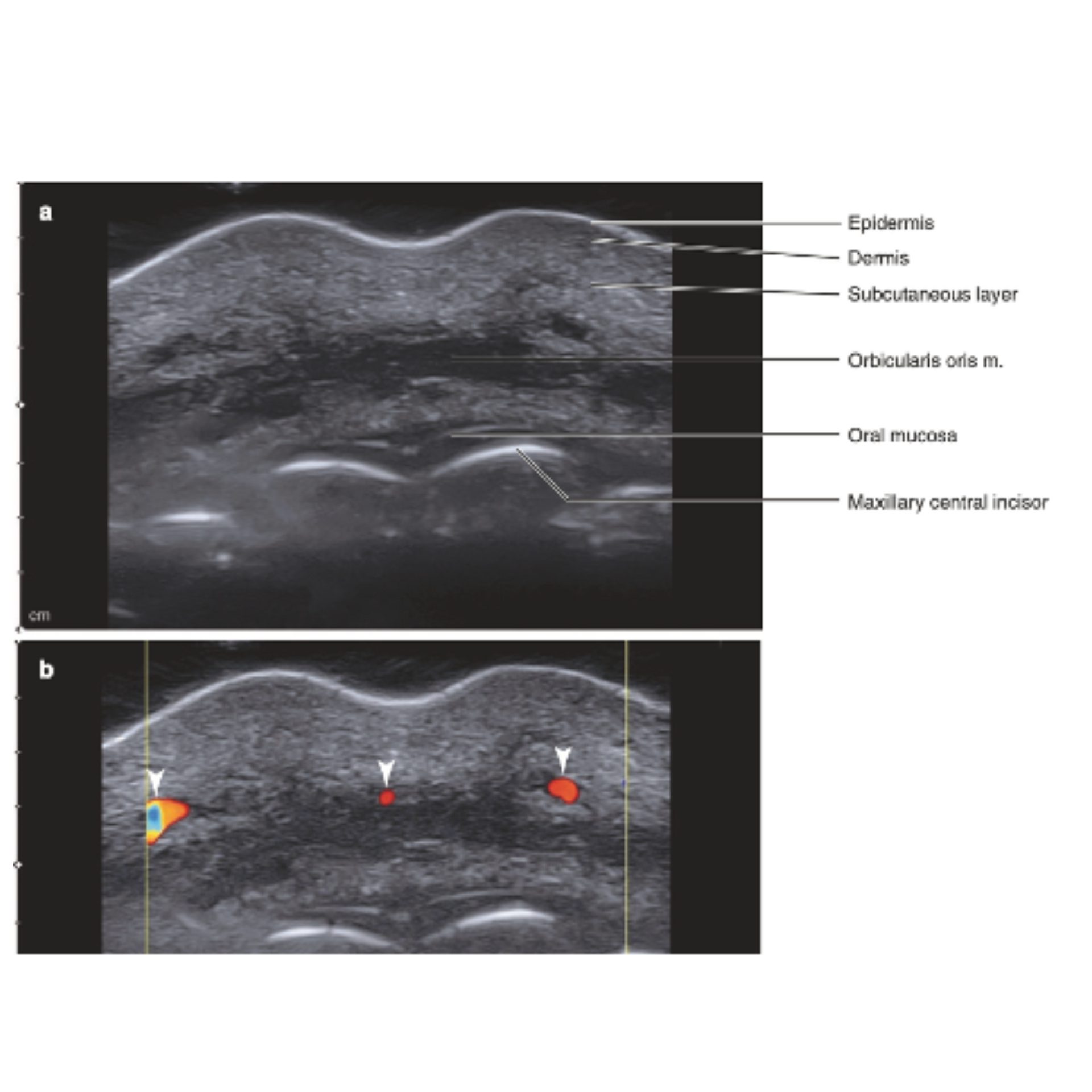
2. Ultrasound must then be used to actively guide the injection of dermal filler into the lips, in real-time (Fig.7). Practitioners can avoid causing vascular occlusion, lumpiness and product migration by directly visualising the injection process to target the correct parts of the lips and avoid danger zones. Additionally, with the greater accuracy of injection afforded by ultrasound guidance, it has been shown that a significantly lower volume of filler can be used to achieve the desired clinical result, further enhancing treatment safety.
If those two methods are performed appropriately, there should never be a need for the final way in which ultrasound can be used to improve the placement of dermal filler and bring the procedures in line with mainstream healthcare protocols, but it’s nice to know it exists. While the preceding two steps are designed to eliminate the potential for dermal filler complications, should they occur - perhaps in a patient referred by a practitioner who isn’t yet uses ultrasound guidance – the final use for ultrasound is to more accurate diagnose and guide the emergency treatment of complications, like vascular occlusion.
Medications exist which readily facilitate the dissolving of dermal filler in situ when serious complications occur, though they are not without their own side effects and ought to be used sparingly. However previously, when working in a blinded fashion, diagnosing, locating and treating offending masses of filler, especially those causing vascular compromise deep within tissues, was clinically challenging, often requiring blanket, widespread, high dosing of the skin with emergency drugs in the hope of achieving the desired response.
With ultrasound guidance, clinicians are now able to accurately visualise the precise location of complications and blockages, delivering targeted, low dose procedures, with real-time imaging, meaning both the placement and ongoing management of dermal filler, is safer and more effective than ever before (Fig.8).
What more do Dentists need to know?
Until now, Dentists had no other option but to inject dermal filler in a blinded fashion and this was the old accepted clinical standard which is now out-dated. In order to continue providing facial injections of Botox and Dermal Filler, Dentists need to undergo training in how to utilise AADFA’s ultrasound protocols for increased safety and efficacy. As the use of ultrasound technology is not a regulated procedure, it is wise for Dentists to ensure their assisting staff members are also fluent in the use of the technology, as this allows for greater clinical efficiency in practice.
While the ability to offer safer procedures under ultrasound guidance also creates a marketable point-of-difference for leading practitioners, those who remain unable to utilise ultrasound protocols for dermal filler lip injections, would now be expected to refer to someone who can.
Article references available by emailing: clinical@AADFA.net